My recent article on carbs covered the carb basics including what they are, different types of carbs and current guidelines on carbs and sugar consumption. And last but not least why we actually NEED them. But I decided to extend this carb talk. In this article we’ll dig a bit deeper to learn what glycemic index actually means, what are its benefits and limitations and whether it can help prevent type 2 diabetes and insulin resistance.
What is the glycemic index
The glycemic index might seem really confusing and hard to interpret. The glycemic index (GI) reflects the capacity of a carb food to affect blood sugar level. We can translate it trough a number from 0 to 100 depending on how much this food raises blood glucose. The GI is divided into 3 groups: low GI from 0 to 55, moderate from 56 to 69 and high GI is over 70.
In order to fully understand it, let’s see how it’s defined. The GI of all carb foods is determined by comparing them to a reference GI of 100 assigned to pure glucose (and not saccharose or table sugar). Very technically speaking (sorry!), the GI is a number which reflects a rise of blood glucose after ingesting a food with 50 g of carbs in the two following hours. The obtained GI is an average result from 10 healthy participants. There are multiple GI databases but the most well-known and reliable one is the GI database of the University of Sydney (1).
Here are a few examples of some common carb foods:
Low Glycemic index
- Apple +/- 30
- Carrot, raw 16
- Canned beans, baked 40
Moderate glycemic index
- Wholewheat pasta, boiled 58
- Basmati rice, cooked +/-60
- Pasta, boiled 61
High glycemic index
- Bread (French baguette) +/- 80
- Desiree potato, peeled, boiled 35 min – 101
GI is a complex concept, to make it a little easier it is often represented with the help of a graph. The graph below illustrates blood glucose flactuation after ingestion a low-GI food versus a high-GI food. A low-GI food makes a modest and smooth blood glucose raise and drop, whereas a high-GI makes blood sugar rise significantly leading to a sudden drop that goes under the starting blood glucose level.
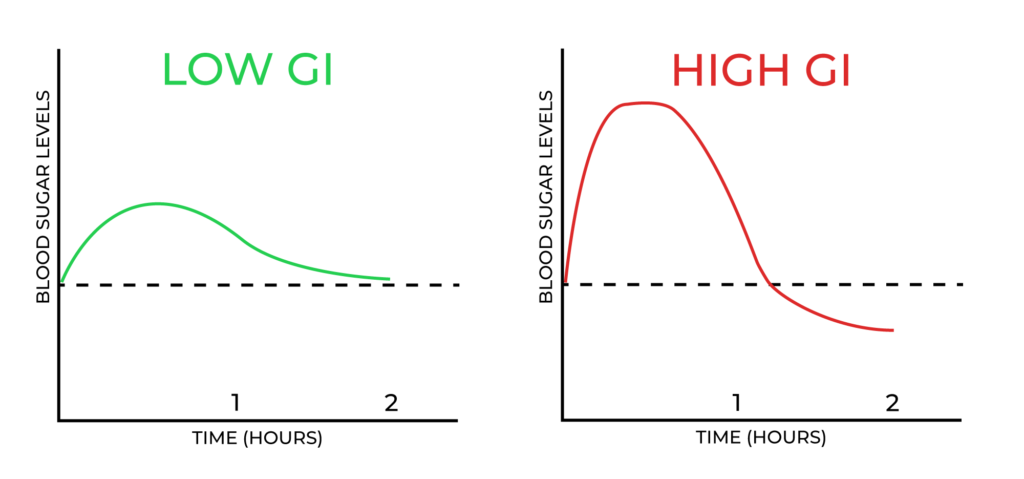
GI, hunger and cravings
I learnt in my French school that the graph above explains exactly why high-GI diet leads to increased hunger and cravings. According to this theory, this very drastic blood sugar drop after eating a high-carb food is the one to blame for extra hunger and a vicious sugar craving circle. Even though this theory seems logical, it is actually oversimplified and has not been proven in clinical trials. It might also be due to the fact that low-GI foods are often richer in fiber, and we know that fiber increases satiety.
Glycemic index limitations and glycemic load
There’s been a lot of fuss around GI. Nowadays, some research doesn’t find it conclusive to use GI since each person’s reaction to a certain food may vary greatly. Nonetheless, in my opinion it allows to have an idea of how a specific food will affect blood sugar. There are different databases that can have different GI results but usually they belong to the same group (low/medium/high).
The main reason we should be more careful with GI is that it doesn’t take into account the nutritional value of the food. For example, ice cream has a lower GI (+/-60) than melon (70). But melon is rich in fiber and vitamins, when ice cream is often full of added sugar and fat, so it remains an occasional dessert. Also it’s very rare that we consume just one food separately, usually we have a meal with several different foods and unfornunately GI is applicable only to isolated foods.
Another downside of the glycemic index is the fact that it doesn’t take into acount the amount of ingested carbs. That’s why a term glycemic load has been invented. Glycemic load (GL) is a more recent method that estimates the blood sugar raise after ingesting a certain carb food. The glycemic load is also represented with a number.
The main difference is that it DOES take into account the amount of carbs in the food. We can calculate glycemic load of a food based on its glycemic index: GI*amount of carbs/100. From 0-10 it’s a low glycemic load, from 10 to 20 – medium and over 20 – high. For example, a serving size of a melon is 120 g and it contains just 6 g of carbohydrates per serving, so 70*(6)/100= 4, which makes it a low glycemic load. A 100 g serving of ice cream will have a glycemic load of 17, which is clearly much higher.
GI health benefits and weight management
Mantaining a low GI diet has shown some promising results in managing and preventing type 2 diabetes. A meta analysis of 54 randomized controlled trials suggests that low-GI diets may be useful for glycemic control and may reduce body weight in people with prediabetes or diabetes (2). Another study concluded that participants who consumed a combination diet that was high in glycemic index or glycemic load and low in cereal fiber had an ∼50% higher risk of developing type 2 diabetes (3).
Does a low-GI diet help lose weight? There is not much conclusive research on this topic. A randomized 2014 study suggests that “A low-GI and energy-restricted diet containing moderate amounts of carbohydrates may be more effective than a high-GI and low-fat diet at reducing body weight and controlling glucose and insulin metabolism” (4).
So, the question is, does it make sense at all to mantain a low-GI diet? In my opinion a balanced diet rich in fiber and based on whole foods is more sustainable and effective than a classic low-GI diet. Knowing that there are multiple factors that lower GI/GL of a meal, I’d like to share with you some tips on how to have a sustainable diet which will be low-moderate GI/GL by default.
How to have a lower GI diet without knowing the GI of foods?

- Prioritize whole-grains (whole-wheat bread, pasta, brown rice, quinoa, etc.) They contain more valuable fiber and their GI/GL is lower.
- Balance your meals. If you associate a carb food with a source of fiber, protein and fat, then glucose will be absorbed more slowly and the GI of the whole meal will descrease. For example, instead of having pasta with tomato sauce, try having pasta with tomato sauce and protein (for example, shrimp or chicken) and a small salad with olive oil as an appetizer (fiber+fat).
- And what about dessert? No problem, but have it at the end of the meal. We can use the same logic regarding snacks. Minimize pure carb snacks like chocolate bar or white bread. Mix it up instead. Take a fruit + nuts or yoghurt with nuts or some bread with butter and a fruit.
- Don’t overcook starches (pasta al dente tastes better anyway) and go for whole foods (fruit instead of juice, oatmeal instead of cornflakes, simple homemade meal instead of a transformed one with over 30 ingredients).
Practically speaking
Glycemic index is a number from 0 to over 100 assigned to carb foods. It reflects the capacity of these individual foods to raise our blood sugar. Glycemic load (another number from 0 to over 20) is a more recent and accurate evaluation method since it takes into account the amount of ingested carbs. Some studies show that glycemic index/load can be benefitial in preventing and managing type 2 diabetes. But the evidence is not conclusive. The main limitation of a low-GI diet is that it can get really confusing and frustrating. Good news, a balanced diet rich in fiber along with an active lifestyle can be more efficient in preventing type 2 diabetes and obesity than a classic low-GI diet. And last but not least, don’t forget to enjoy your meals!



